Swabian Joint Center
Knee pain is common and occurs in all age groups. The biomechanics of our largest joint are complex and therefore prone to pain. Learn more about your knee joint, the typical causes of pain and what you can do.
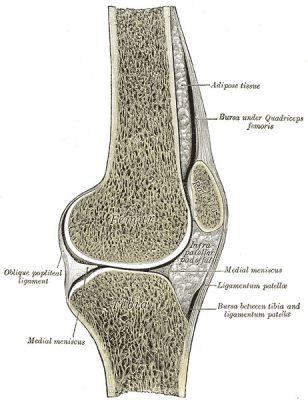
The knee - A biomechanical unit of 3 partial joints
The knee joint is the largest joint in the human body and consists of 3 partial joints.
A partial joint of the knee is located on the inner side and a partial joint on the outer side between the thigh and lower leg bones. Another partial joint is located behind the kneecap. The joint forming surfaces are covered by hyaline cartilage.
The knee joint is a hinge joint with two degrees of rotational freedom. It can bend and stretch in the lateral plane and rotate inward and outward in the horizontal plane when bent.
The kneecap (patella) is incorporated as a sesamoid bone into the insertion tendon of the four-headed thigh muscle (Musculus quadriceps femoris). The patella increases the effectiveness of the quadriceps tendon and reduces the load on the knee joint.

- The stability of the knee joint is ensured by a tight capsule-ligament apparatus, consisting of the actual joint capsule, the extensor apparatus, the collateral ligament apparatus, the posterior ligament apparatus and the central ligament complex.
- The anterior and posterior cruciate ligaments provide stability to the knee joint during movement by limiting rotational movements, especially the internal rotation of the lower leg relative to the thigh. In this way, the cruciate ligaments prevent the knee joint from over-rotating inwards by wrapping both ligaments around each other during this movement. The cruciate ligaments also prevent overstretching, i.e. excessive bending and stretching of the knee.
Cruciate ligaments

- The cause of cruciate ligament injuries such as cruciate ligament tears is often sports accidents.
- Cruciate ligament injuries are very painful.
- A distinction is made between the following forms of cruciate ligament injury: cruciate ligament rupture, cruciate ligament tear, cruciate ligament extension.
- An examination by the cruciate ligament specialist is recommended to assess the stability of the cruciate ligaments and to be able to initiate the right therapy depending on the type of injury.
- The sports physicians of the SGZ are specialized in the treatment of cruciate ligament injuries.
- The classic accident mechanism for cruciate ligament injuries is when the knee is involuntarily overextended, forced into a knock-knee position or twisted outwards.
- Either with external influence, e.g. when tackling in football or ice hockey, or very often accidents without external influence, such as when skiing in the Alps, or even bending over when landing after jumps or after stumbling.
The anterior cruciate ligament generally carries a greater weight than the posterior cruciate ligament and is therefore more frequently injured.
- In case of extreme violence, for example in traffic accidents, the rear cruciate ligament tears.
- In addition, accompanying injuries such as torn collateral ligaments, meniscus and cartilage injuries can occur. Chronic instabilities usually end in gonarthrosis.
- Instability that is not treated leads to chronic instability and, due to the altered biomechanics, to an unphysiological load on the internal structures of the knee.
- Secondary damage is the result.
- In the long term, cartilage wear and the development of knee arthrosis (gonarthrosis) often occurs.
- Pain and feeling of pressure in the knee joint caused by the bruise.
- Restriction of movement and loss of stability with uncertainty when walking.
- One has the feeling that one can no longer rely on the knee.
- With the help of X-rays of the knee joint, the bone structure in the knee joint can be assessed and bony ligament ruptures can be diagnosed.
- In addition, special X-ray stress images of the knee can detect ligament injuries.
- Magnetic resonance tomography (MRT) is the method of choice for visualizing all structures in the knee joint and diagnosing torn cruciate ligaments.
- Knee endoscopy (arthroscopy) enables SGZ knee specialists to use an instrument to make small incisions to directly examine the cruciate ligament for stability and to carry out therapy directly in the event of injury.
- A torn cruciate ligament does not always have to be operated on immediately.
- It is crucial that even conservative therapy restores sufficient stability to the knee joint.
- Conservative therapy means trying to restore the stability of the knee joint with the help of physiotherapy, bandages and orthoses.
- The disadvantage of conservative therapy is that patients often have to accept a reduction in physical and thus sporting activity.
- Our young, adolescent patients and sporty, active people are usually treated surgically in case of a cruciate ligament rupture, since their knee joint particularly needs the stabilizing function of the anterior cruciate ligament.
- For this reason, the indication for surgery for cruciate ligament rupture is discussed in detail with the patient and his or her needs at the SGZ in order to find the best solution for each individual patient.
- The surgical therapy is performed arthroscopically and with a small incision (mini-open).
- The cruciate ligament specialists at the SGZ have mastered all techniques of cruciate ligament surgery.
- This means that both recreational and competitive athletes (e.g. professional footballers) as well as children with open growth joints can be optimally treated with cruciate ligament surgery at the SGZ.
- Each patient is considered individually according to the SGZ philosophy and is accordingly provided with the ideal cruciate ligament replacement.
- The cruciate ligament operation is performed when the knee is swollen and mobile again after the accident.
- This minimizes the risk of massive connective tissue formation (arthrofibrosis) with restricted movement.
- After the cruciate ligament operation, the knee should only be partially loaded with 20 kg for 2 weeks.
- Afterwards, the load is increased depending on the pain and under physiotherapeutic guidance, and if the patient has good mobility, cycling on the ergometer can be started.
- The knee orthosis should be worn for 6 weeks with released mobility.
- This is followed by muscle building and coordination training. Swimming is now permitted again.
- Important: Remember to take thrombosis prophylaxis until a fluid gait pattern is achieved.
- If the healing process is regular, jogging may be started again after 3 months in consultation with your surgeon.
- Contact sports such as football, ice hockey, handball, basketball, are not recommended until 6-8 months after the operation.
- The cause of cruciate ligament injuries such as cruciate ligament tears is often sports accidents.
- Cruciate ligament injuries are very painful.
- A distinction is made between the following forms of cruciate ligament injury: cruciate ligament rupture, cruciate ligament tear, cruciate ligament extension.
- An examination by the cruciate ligament specialist is recommended to assess the stability of the cruciate ligaments and to be able to initiate the right therapy depending on the type of injury.
- The sports physicians of the SGZ are specialized in the treatment of cruciate ligament injuries.
- The classic accident mechanism for cruciate ligament injuries is when the knee is involuntarily overextended, forced into a knock-knee position or twisted outwards.
- Either with external influence, e.g. when tackling in football or ice hockey, or very often accidents without external influence, such as when skiing in the Alps, or even bending over when landing after jumps or after stumbling.
- The anterior cruciate ligament generally carries a greater weight than the posterior cruciate ligament and is therefore more frequently injured.
- In case of extreme violence, for example in traffic accidents, the rear cruciate ligament tears.
- In addition, accompanying injuries such as torn collateral ligaments, meniscus and cartilage injuries can occur. Chronic instabilities usually end in gonarthrosis.
- Instability that is not treated leads to chronic instability and, due to the altered biomechanics, to an unphysiological load on the internal structures of the knee.
- Secondary damage is the result.
- In the long term, cartilage wear and the development of knee arthrosis (gonarthrosis) often occurs.
- Pain and feeling of pressure in the knee joint caused by the bruise.
- Restriction of movement and loss of stability with uncertainty when walking.
- One has the feeling that one can no longer rely on the knee.
- With the help of X-rays of the knee joint, the bone structure in the knee joint can be assessed and bony ligament ruptures can be diagnosed.
- In addition, special X-ray stress images of the knee can detect ligament injuries.
- Magnetic resonance tomography (MRT) is the method of choice for visualizing all structures in the knee joint and diagnosing torn cruciate ligaments.
- Knee endoscopy (arthroscopy) enables SGZ knee specialists to use an instrument to make small incisions to directly examine the cruciate ligament for stability and to carry out therapy directly in the event of injury.
- A torn cruciate ligament does not always have to be operated on immediately.
- It is crucial that even conservative therapy restores sufficient stability to the knee joint.
- Conservative therapy means trying to restore the stability of the knee joint with the help of physiotherapy, bandages and orthoses.
- The disadvantage of conservative therapy is that patients often have to accept a reduction in physical and thus sporting activity.
- Our young, adolescent patients and sporty, active people are usually treated surgically in case of a cruciate ligament rupture, since their knee joint particularly needs the stabilizing function of the anterior cruciate ligament.
- For this reason, the indication for surgery for cruciate ligament rupture is discussed in detail with the patient and his or her needs at the SGZ in order to find the best solution for each individual patient.
- The surgical therapy is performed arthroscopically and with a small incision (mini-open).
- The cruciate ligament specialists at the SGZ have mastered all techniques of cruciate ligament surgery.
- This means that both recreational and competitive athletes (e.g. professional footballers) as well as children with open growth joints can be optimally treated with cruciate ligament surgery at the SGZ.
- Each patient is considered individually according to the SGZ philosophy and is accordingly provided with the ideal cruciate ligament replacement.
- The cruciate ligament operation is performed when the knee is swollen and mobile again after the accident.
- This minimizes the risk of massive connective tissue formation (arthrofibrosis) with restricted movement.
- After the cruciate ligament operation, the knee should only be partially loaded with 20 kg for 2 weeks.
- Afterwards, the load is increased depending on the pain and under physiotherapeutic guidance, and if the patient has good mobility, cycling on the ergometer can be started.
- The knee orthosis should be worn for 6 weeks with released mobility.
- This is followed by muscle building and coordination training. Swimming is now permitted again.
- Important: Remember to take thrombosis prophylaxis until a fluid gait pattern is achieved.
- If the healing process is regular, jogging may be started again after 3 months in consultation with your surgeon.
- Contact sports such as football, ice hockey, handball, basketball, are not recommended until 6-8 months after the operation.
Meniscus

- The inner and outer meniscus are shock absorbers at the knee joint which owe their name meniscus (=mountain) to their classical form.
- The menisci are located in the knee joint between the femur and tibia, are an important stabilizer and protect the joint cartilage by acting as shock absorbers.
- A healthy meniscus is nourished by the synovial fluid, the outer part is supplied with blood.
- Both the inner and the outer meniscus can be affected. The inner meniscus is more frequently affected by a meniscus tear than the outer meniscus.
- The cause of the meniscus lesion is either wear and tear or trauma.
- Meniscus lesions cause knee pain and reduced mobility and can cause premature joint wear and tear.
- Pain in the area of the inner or outer knee joint gap during and after loading
- Pain when sitting cross-legged and squatting
- Spontaneously occurring joint blockades in different joint positions (inhibition of extension and flexion)
- Our knee specialists will first take a detailed anamnesis with you to record your individual medical history.
- Special meniscus tests are then used to examine the knee joint in a targeted examination.
- X-rays can be used to visualize wear and tear of the cartilage in the knee.
- Magnetic resonance tomography (MRT) allows an assessment of the type and extent of a torn meniscus.
- The safest diagnostic method of meniscus lesion is arthroscopy (joint endoscopy) of the knee. This means that you as the patient receive an anaesthetic and your surgeon can look into the knee joint through a small minimally invasive incision (approx. 5 mm) with a kind of video camera (optics). Because the incision is hardly visible after the scar has healed, this is also referred to as keyhole technique.
- The advantage of arthroscopy is that your experienced knee surgeon at the SGZ can use arthroscopy to diagnose the meniscus tear and treat it immediately.
- Accompanying damage to the knee joint, which is common in meniscus lesions, can be treated in the same arthroscopic operation.
- Minor and degenerative meniscus injuries.
- In the acute stage of meniscus tears, immobilisation of the knee and local cooling helps.
- Supporting bandages and physiotherapy can provide relief.
- Drugs that have analgesic and anti-inflammatory effects help in the acute phase.
- Hyaluronic acid and autohaemotherapy (ACP) can improve the lubrication of the knee joint.
- During ACP therapy (Autologous Conditioned Plasma), highly concentrated growth factors can support and accelerate the healing process.
- Meniscus tears that become a mechanical problem due to a joint blockage or if chronic pain is present, meniscus surgery may be necessary.
- Then an arthroscopic procedure is indicated to treat the problem.
- The SGZ knee specialists will discuss with you individually which form of therapy will bring the best results for your meniscus problem.
- The inner and outer meniscus are shock absorbers at the knee joint which owe their name meniscus (=mountain) to their classical form.
- The menisci are located in the knee joint between the femur and tibia, are an important stabilizer and protect the joint cartilage by acting as shock absorbers.
- A healthy meniscus is nourished by the synovial fluid, the outer part is supplied with blood.
- Both the inner and the outer meniscus can be affected. The inner meniscus is more frequently affected by a meniscus tear than the outer meniscus.
- The cause of the meniscus lesion is either wear and tear or trauma.
- Meniscus lesions cause knee pain and reduced mobility and can cause premature joint wear and tear.
- Pain in the area of the inner or outer knee joint gap during and after loading
- Pain when sitting cross-legged and squatting
- Spontaneously occurring joint blockades in different joint positions (inhibition of extension and flexion)
- Our knee specialists will first take a detailed anamnesis with you to record your individual medical history.
- Special meniscus tests are then used to examine the knee joint in a targeted examination.
- X-rays can be used to visualize wear and tear of the cartilage in the knee.
- Magnetic resonance tomography (MRT) allows an assessment of the type and extent of a torn meniscus.
- The safest diagnostic method of meniscus lesion is arthroscopy (joint endoscopy) of the knee. This means that you as the patient receive an anaesthetic and your surgeon can look into the knee joint through a small minimally invasive incision (approx. 5 mm) with a kind of video camera (optics). Because the incision is hardly visible after the scar has healed, this is also referred to as keyhole technique.
- The advantage of arthroscopy is that your experienced knee surgeon at the SGZ can use arthroscopy to diagnose the meniscus tear and treat it immediately.
- Accompanying damage to the knee joint, which is common in meniscus lesions, can be treated in the same arthroscopic operation.
- Minor and degenerative meniscus injuries.
- In the acute stage of meniscus tears, immobilisation of the knee and local cooling helps.
- Supporting bandages and physiotherapy can provide relief.
- Drugs that have analgesic and anti-inflammatory effects help in the acute phase.
- Hyaluronic acid and autohaemotherapy (ACP) can improve the lubrication of the knee joint.
- During ACP therapy (Autologous Conditioned Plasma), highly concentrated growth factors can support and accelerate the healing process.
- Meniscus tears that become a mechanical problem due to a joint blockage or if chronic pain is present, meniscus surgery may be necessary.
- Then an arthroscopic procedure is indicated to treat the problem.
- The SGZ knee specialists will discuss with you individually which form of therapy will bring the best results for your meniscus problem.
Patella luxation - Patella luxation
- Patellar luxation (dislocation) is the extreme form of knee instability and a common clinical picture in adolescents.
- The kneecap (patella) has no bony guidance and runs only in a groove of the thigh bone.
- Acute patella luxation is described as pain and a sudden subsidence of the knee.
- Muscular imbalance with a predominance of the external muscle parts (vastus lateralis muscle)
- Connective tissue weakness
- Misalignment of the legs (X-B adjustment)
- Congenital malformation of the patella with a too flat back surface of the patella and the articular surface of the thigh (hypo- or dysplastic)
- As a result of an accident or dislocation of the kneecap, the inner knee retaining ligament (= MPFL - Medial Patello Femoral Ligament) tears, causing instability
- Patients with patellar instability usually suffer from pain in the front part of the joint.
- The pain is typically more pronounced when going downhill.
- Often a deformation of the knee is visible, with the patella being displaced towards the outside.
- The knee is protected in the bent position, the mobility of the knee joint is limited.
- A joint effusion causes pressure sensitivity.
- Dislocation of the patella can occur repeatedly.
- Our knee specialists will first take a detailed anamnesis with you to record your individual medical history.
- Special patellar tests are then used to examine the affected muscles, tendons and ligaments in a targeted examination. The examination can also be used to detect swelling, effusion and axial deviation.
- In addition, an ultrasound examination is often carried out, whereby muscles, ligaments and a joint effusion can be imaged.
- It is important to distinguish more harmless problems in the growth phase from serious instabilities and imbalances.
- X-rays and magnetic resonance tomography (MRT) are used to make injuries visible.
- The initial luxation of the patella can be treated conservatively, if no severe pathology is present.
- The aim of the therapy is to restore full resilience in everyday life and sports and to prevent a renewed luxation.
- After initial immobilization with a patellar stabilizing knee orthosis, the inner muscle group (vastus medialis muscle) is strengthened to stabilize the patella.
- After a second dislocation, the risk of a renewed dislocation is about 50% and in the case of chronic instability, surgical therapy is performed to stabilize and prevent consequential damage to the joint cartilage.
- Depending on the pathology, the operation consists of different sub-steps.
- The reconstruction of the medial knee retaining ligament (MPFL), the most important passive stabilizer of the knee joint, is often decisive.
- This ensures an optimal hold of the kneecap in extension and flexion.
- If cartilage is detached, arthroscopic treatment of the cartilage damage is necessary.
- In the first phase after the operation, muscle building is the central point of the therapy.
- Stronger flexion is possible after 6 weeks.
- Complete healing can be expected after approx. 3 months.
- Patellar luxation (dislocation) is the extreme form of knee instability and a common clinical picture in adolescents.
- The kneecap (patella) has no bony guidance and runs only in a groove of the thigh bone.
- Acute patella luxation is described as pain and a sudden subsidence of the knee.
- Muscular imbalance with a predominance of the external muscle parts (vastus lateralis muscle)
- Connective tissue weakness
- Misalignment of the legs (X-B adjustment)
- Congenital malformation of the patella with a too flat back surface of the patella and the articular surface of the thigh (hypo- or dysplastic)
- As a result of an accident or dislocation of the kneecap, the inner knee retaining ligament (= MPFL - Medial Patello Femoral Ligament) tears, causing instability
- Patients with patellar instability usually suffer from pain in the front part of the joint.
- The pain is typically more pronounced when going downhill.
- Often a deformation of the knee is visible, with the patella being displaced towards the outside.
- The knee is protected in the bent position, the mobility of the knee joint is limited.
- A joint effusion causes pressure sensitivity.
- Dislocation of the patella can occur repeatedly.
- Our knee specialists will first take a detailed anamnesis with you to record your individual medical history.
- Special patellar tests are then used to examine the affected muscles, tendons and ligaments in a targeted examination. The examination can also be used to detect swelling, effusion and axial deviation.
- In addition, an ultrasound examination is often carried out, whereby muscles, ligaments and a joint effusion can be imaged.
- It is important to distinguish more harmless problems in the growth phase from serious instabilities and imbalances.
- X-rays and magnetic resonance tomography (MRT) are used to make injuries visible.
- The initial luxation of the patella can be treated conservatively, if no severe pathology is present.
- The aim of the therapy is to restore full resilience in everyday life and sports and to prevent a renewed luxation.
- After initial immobilization with a patellar stabilizing knee orthosis, the inner muscle group (vastus medialis muscle) is strengthened to stabilize the patella.
- After a second dislocation, the risk of a renewed dislocation is about 50% and in the case of chronic instability, surgical therapy is performed to stabilize and prevent consequential damage to the joint cartilage.
- Depending on the pathology, the operation consists of different sub-steps.
- The reconstruction of the medial knee retaining ligament (MPFL), the most important passive stabilizer of the knee joint, is often decisive.
- This ensures an optimal hold of the kneecap in extension and flexion.
- If cartilage is detached, arthroscopic treatment of the cartilage damage is necessary.
- In the first phase after the operation, muscle building is the central point of the therapy.
- Stronger flexion is possible after 6 weeks.
- Complete healing can be expected after approx. 3 months.
Cartilage damage
- In a joint, bones are movably connected to each other. The contact surfaces of the bones are covered with cartilage tissue.
- Cartilage has no nerves or pain fibers, which is why we can move without pain. However, this is also why cartilage only tells us very late when it is damaged.
- The cartilage tissue consists of avascular supporting tissue and chondrocytes (cartilage cells), which form collagen fibres that are cross-linked with each other. A large amount of water can be bound between the fibres, which enables pressure elasticity and protects against pressure loads.
- There are no blood vessels in the cartilage, so the supply of nutrients takes place through the cartilage skin and the synovial fluid.
- Cartilage damage is either caused by an accident, such as a sports injury, or degenerative as a result of incorrect loading, overweight and recurring micro injuries.
- The cartilage itself is not sensitive to pain, i.e. minor cartilage damage does not immediately trigger pain as an alarm signal.
- Pain is only caused by accompanying damage or when the cartilage is completely and extensively destroyed and rubs bone on bone.
- Therefore, early detection is important so that corrective knee joint therapies can be initiated while cartilage substance is still present.
- Cartilage damage often results in swelling of the knee, which, in addition to pain, restricts the range of movement.
- For the detection of early damage, magnetic resonance imaging (MRI) is the method of choice.
- With the help of conservative therapy, the further course of knee arthrosis with cartilage damage can be favourably influenced.
- Weight normalization and knee-sparing physical activity with training of the joint-spanning musculature are essential basics of conservative therapy.
- Shoe insoles, bandages and orthoses can improve the symptoms.
- In conservative therapy, success is achieved with movement therapy, strengthening therapy, electrotherapy, heat or cold applications and also acupuncture.
- In the case of advanced knee arthrosis, targeted injections of cortisone into the focus of inflammation can relieve the pain.
- In the surgical therapy of circumscribed cartilage damage, the size of the cartilage damage is determined by means of arthroscopy and the defect is filled with cartilage replacement tissue.
- In the case of additional biomechanical pathologies such as pronounced O or X leg malposition, a leg axis correction is additionally performed to reduce the load on the damaged joint section and thus improve the chances of recovery.
- Microfracturing involves drilling small holes in the defect zone in order to stimulate the exit of stem cells from the bone into the cartilage defect. These stem cells can regenerate replacement cartilage tissue in the vicinity of healthy cartilage.
- Microfracturing can be combined with a collagen matrix or the application of hyaluronic acid, which can improve the results.
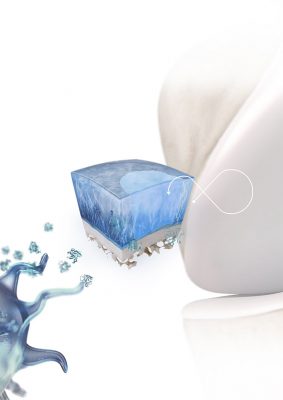
- Under optimal conditions, various techniques can lead to successful tissue formation
- This requires cells that can regenerate, a matrix in which they can grow, and growth factors that act as biological signal molecules and control the growth process.
- In cartilage cell transplantation, cartilage cells are removed from an unimportant part of the joint in an initial arthroscopic operation.
- In a special cell culture process, small spheroidal bodies (spheroids) are formed from the removed cartilage cells without the addition of foreign substances, enclosing up to 200,000 cartilage cells per sphere.
- After about 6 weeks, the spheroids that have now formed are inserted into the cartilage defect zone in a second arthroscopic operation, adhere there independently and form a cartilage replacement tissue that has similar biomechanical properties to the original cartilage.
- In the best case, the cartilage replacement tissue combines with the healthy cartilage at the edge of the defect.
- The first 6 weeks should be relieved, after that the partial weight bearing starts.
- After 3 months, the partially regenerated cartilage surface can carry the body weight, which is why gentle sports such as cycling and swimming can then be practised again.
- Complete healing and regeneration of the new cartilage can be expected after 1 year.
- In a joint, bones are movably connected to each other. The contact surfaces of the bones are covered with cartilage tissue.
- Cartilage has no nerves or pain fibers, which is why we can move without pain. However, this is also why cartilage only tells us very late when it is damaged.
- The cartilage tissue consists of avascular supporting tissue and chondrocytes (cartilage cells), which form collagen fibres that are cross-linked with each other. A large amount of water can be bound between the fibres, which enables pressure elasticity and protects against pressure loads.
- There are no blood vessels in the cartilage, so the supply of nutrients takes place through the cartilage skin and the synovial fluid.
- Cartilage damage is either caused by an accident, such as a sports injury, or degenerative as a result of incorrect loading, overweight and recurring micro injuries.
- The cartilage itself is not sensitive to pain, i.e. minor cartilage damage does not immediately trigger pain as an alarm signal.
- Pain is only caused by accompanying damage or when the cartilage is completely and extensively destroyed and rubs bone on bone.
- Therefore, early detection is important so that corrective knee joint therapies can be initiated while cartilage substance is still present.
- Cartilage damage often results in swelling of the knee, which, in addition to pain, restricts the range of movement.
- For the detection of early damage, magnetic resonance imaging (MRI) is the method of choice.
- With the help of conservative therapy, the further course of knee arthrosis with cartilage damage can be favourably influenced.
- Weight normalization and knee-sparing physical activity with training of the joint-spanning musculature are essential basics of conservative therapy.
- Shoe insoles, bandages and orthoses can improve the symptoms.
- In conservative therapy, success is achieved with movement therapy, strengthening therapy, electrotherapy, heat or cold applications and also acupuncture.
- In the case of advanced knee arthrosis, targeted injections of cortisone into the focus of inflammation can relieve the pain.
- In the surgical therapy of circumscribed cartilage damage, the size of the cartilage damage is determined by means of arthroscopy and the defect is filled with cartilage replacement tissue.
- In the case of additional biomechanical pathologies such as pronounced O or X leg malposition, a leg axis correction is additionally performed to reduce the load on the damaged joint section and thus improve the chances of recovery.
- Microfracturing involves drilling small holes in the defect zone in order to stimulate the exit of stem cells from the bone into the cartilage defect. These stem cells can regenerate replacement cartilage tissue in the vicinity of healthy cartilage.
- Microfracturing can be combined with a collagen matrix or the application of hyaluronic acid, which can improve the results.
- Under optimal conditions, various techniques can lead to successful tissue formation
- This requires cells that can regenerate, a matrix in which they can grow, and growth factors that act as biological signal molecules and control the growth process.
- In cartilage cell transplantation, cartilage cells are removed from an unimportant part of the joint in an initial arthroscopic operation.
- In a special cell culture process, small spheroidal bodies (spheroids) are formed from the removed cartilage cells without the addition of foreign substances, enclosing up to 200,000 cartilage cells per sphere.
- After about 6 weeks, the spheroids that have now formed are inserted into the cartilage defect zone in a second arthroscopic operation, adhere there independently and form a cartilage replacement tissue that has similar biomechanical properties to the original cartilage.
- In the best case, the cartilage replacement tissue combines with the healthy cartilage at the edge of the defect.
- The first 6 weeks should be relieved, after that the partial weight bearing starts.
- After 3 months, the partially regenerated cartilage surface can carry the body weight, which is why gentle sports such as cycling and swimming can then be practised again.
- Complete healing and regeneration of the new cartilage can be expected after 1 year.
Knee arthrosis - Gonarthrosis

- Knee arthrosis (gonarthrosis) means that there has been wear and tear of the joint cartilage at the knee joint.
- As a result, bone rubs against bone, causing painful inflammation. Increasing changes in the joint lead to painful restriction of movement.
- Further causes of knee arthrosis are malpositioning of the legs (knock-knees and bow legs) with incorrect loading, rheumatism, fractures near the knee joint and high loads as in top athletes.
- With pronounced bow legs the arthrosis occurs mainly on the inside, with pronounced bow legs on the outside.
- The partial joint behind the kneecap can also be affected by knee arthrosis in isolation.
- The entire knee joint can be affected by the arthrosis (pangon arthrosis).
- At the beginning of the knee arthrosis disease, the joints often hurt only when moving, later also when resting.
- In the course of the disease there are increasing restrictions of movement and recurring swelling.
- Muscle tension, feelings of instability and joint grinding (crepitus) are typical signs of knee arthrosis.
- The detailed anamnesis by the experienced knee specialist provides groundbreaking information on knee arthrosis and its cause.
- Afterwards, a physical examination is carried out at the SGZ. Swelling, effusion, axial deviation and instability of the knee can be detected during the examination.
- In addition, an ultrasound examination is often carried out, whereby muscles, ligaments and joint effusion can be imaged.
- If there is any suspicion, special x-rays are then taken, with the help of which the exact extent of the arthrosis and a malposition can be diagnosed.
- With the help of conservative therapy, the further course of knee arthrosis can be influenced favourably.
- Weight normalization and knee-sparing sports activities such as cycling are essential basics of conservative therapy.
- In conservative therapy, success is achieved with movement therapy, strengthening therapy, electrotherapy, heat or cold applications and also acupuncture.
- In the case of advanced knee arthrosis, targeted injections of cortisone into the focus of inflammation can relieve the pain.
- Hyaluronic acid and autohaemotherapy (ACP) can improve the lubrication of the knee joint.
- Surgery is required when there has been final wear and tear in the knee joint and conservative therapy no longer provides relief.
- A pronounced loss of function with complete loss of the ability to carry out the activities of daily life and bony deformities with axial malformations make surgery necessary.
- Your individual level of suffering is decisive for the right time of operation.
- In surgical treatment, a distinction is made between two types of prosthesis, which can be used depending on the type of knee arthrosis:
- Partial joint replacement: Corresponding to the 3 partial joints at the knee joint, each part can be replaced separately, which means that there is a half-sided prosthesis on the inside or outside (unicondylar joint replacement = sled prosthesis) and the joint surface behind the kneecap can also be replaced in isolation (isolated retropatellar replacement).
- The exact clarification prior to the operation is decisive here, as otherwise the results of the partial joint replacement may be poor. However, excellent results can be expected if the indication is correct.
- In cases of pronounced wear and tear of several compartments of the knee joint, a complete joint replacement (bicondylar joint replacement with patellar back surface replacement) must often be carried out.
- Follow-up treatment begins on the day of the operation and is intensified during the 4-day inpatient stay.
- Early mobilisation helps to strengthen the muscles surrounding the knee joint. Daily activities such as gait training and climbing stairs are integrated into the rehabilitation programme during the inpatient stay.
- Knee arthrosis (gonarthrosis) means that there has been wear and tear of the joint cartilage at the knee joint.
- As a result, bone rubs against bone, causing painful inflammation. Increasing changes in the joint lead to painful restriction of movement.
- Further causes of knee arthrosis are malpositioning of the legs (knock-knees and bow legs) with incorrect loading, rheumatism, fractures near the knee joint and high loads as in top athletes.
- With pronounced bow legs the arthrosis occurs mainly on the inside, with pronounced bow legs on the outside.
- The partial joint behind the kneecap can also be affected by knee arthrosis in isolation.
- The entire knee joint can be affected by the arthrosis (pangon arthrosis).
- At the beginning of the knee arthrosis disease, the joints often hurt only when moving, later also when resting.
- In the course of the disease there are increasing restrictions of movement and recurring swelling.
- Muscle tension, feelings of instability and joint grinding (crepitus) are typical signs of knee arthrosis.
- The detailed anamnesis by the experienced knee specialist provides groundbreaking information on knee arthrosis and its cause.
- Afterwards, a physical examination is carried out at the SGZ. Swelling, effusion, axial deviation and instability of the knee can be detected during the examination.
- In addition, an ultrasound examination is often carried out, whereby muscles, ligaments and joint effusion can be imaged.
- If there is any suspicion, special x-rays are then taken, with the help of which the exact extent of the arthrosis and a malposition can be diagnosed.
- With the help of conservative therapy, the further course of knee arthrosis can be influenced favourably.
- Weight normalization and knee-sparing sports activities such as cycling are essential basics of conservative therapy.
- In conservative therapy, success is achieved with movement therapy, strengthening therapy, electrotherapy, heat or cold applications and also acupuncture.
- In the case of advanced knee arthrosis, targeted injections of cortisone into the focus of inflammation can relieve the pain.
- Hyaluronic acid and autohaemotherapy (ACP) can improve the lubrication of the knee joint.
- Surgery is required when there has been final wear and tear in the knee joint and conservative therapy no longer provides relief.
- A pronounced loss of function with complete loss of the ability to carry out the activities of daily life and bony deformities with axial malformations make surgery necessary.
- Your individual level of suffering is decisive for the right time of operation.
- In surgical treatment, a distinction is made between two types of prosthesis, which can be used depending on the type of knee arthrosis:
- Partial joint replacement: Corresponding to the 3 partial joints at the knee joint, each part can be replaced separately, which means that there is a half-sided prosthesis on the inside or outside (unicondylar joint replacement = sled prosthesis) and the joint surface behind the kneecap can also be replaced in isolation (isolated retropatellar replacement).
- The exact clarification prior to the operation is decisive here, as otherwise the results of the partial joint replacement may be poor. However, excellent results can be expected if the indication is correct.
- In cases of pronounced wear and tear of several compartments of the knee joint, a complete joint replacement (bicondylar joint replacement with patellar back surface replacement) must often be carried out.
- Follow-up treatment begins on the day of the operation and is intensified during the 4-day inpatient stay.
- Early mobilisation helps to strengthen the muscles surrounding the knee joint. Daily activities such as gait training and climbing stairs are integrated into the rehabilitation programme during the inpatient stay.
