Swabian Joint Center
The shoulder as the most flexible joint in our body is susceptible to pain. Every tenth person complains of shoulder pain. The complaints are often excruciating and restrict those affected for a long time. Here you can learn more about the special features of your shoulder joints, the typical causes of pain and what you can do to get rid of them.
Shoulder - a special joint
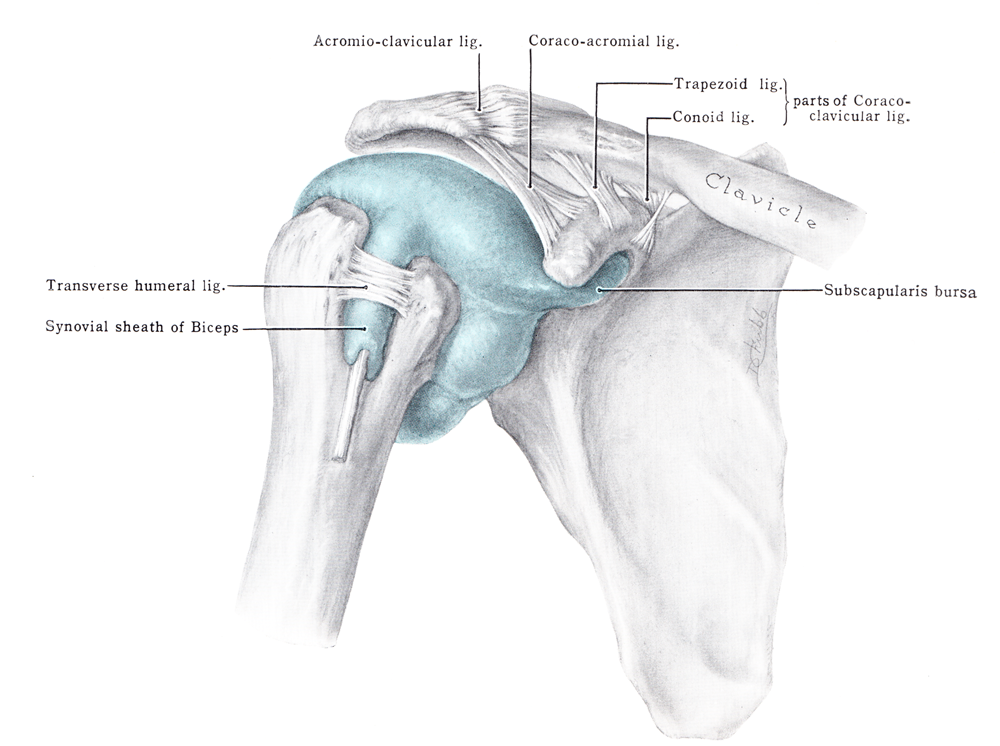
The large radius of movement that our hand needs for optimal use is ensured by the design of the arm as a joint chain and the special mobility of the shoulder joint (glenohumeral joint) and the shoulder girdle.
The performance of this functional unit "shoulder" is achieved through the complex structure of the capsule-ligament apparatus and differentiated neuromuscular control.
The mechanics of the shoulder joint is more complex than in other human joints, since the small socket means that a balance between stability and mobility must be constantly found.
" Shoulder pain - your shoulder problem
Shoulder pain often leads to a significant reduction in quality of life due to poor mobility, loss of strength, pain resistant to therapy and disturbed night's sleep. Many shoulder patients have experience with conservative or operative therapy measures, without these having contributed to a long-term improvement of the situation.
Here at the SGZ the specialized shoulder team around Professor Dr. Michael Maier will be happy to help you.
Rotator cuff

- The end tendons of 4 connected muscles, which surround the head of humerus like a cuff, are called rotator cuffs.
- The muscles of the rotator cuff move from the shoulder blade to the head of humerus and attach their tendons there. The muscles involved are as follows: Subscapular, supraspinatus, infraspinatus and teres minor.
- The rotator cuff cannot be palpated because it is located deep below the shoulder cap muscle (deltoid muscle).
- The rotator cuff stabilises the head of humerus in the small socket at the shoulder joint and is therefore an essential component of pain-free mobility of the upper arm in the shoulder joint.
- For stabilization at the shoulder joint, the strength of a well-trained rotator cuff musculature is required, which is why the shoulder is also referred to as a "friction-locked" joint.
- According to its name, the rotator cuff is responsible for the rotational movement in the shoulder joint in terms of internal and external rotation. A balance of force couples is crucial for pain-free shoulder function.
- A traumatic event or wear and tear due to excessive stress can cause a tear of one or more tendons of the rotator cuff. As a result, the function of the entire shoulder is often impaired.
- The frequency of rotator cuff lesions increases with age.
- The tendons, some of which are overstressed by inflammation, tear, fray and form defects that grow larger and larger.
- In younger people, the most common cause is an accident, in older people degenerative changes in the cuff that lead to a tear.
- If the rotator cuff tendon tears, the supraspinatus tendon is most frequently affected.
- If these defects are diagnosed in time, they can be sutured. If left untreated, the defects often increase further, and regression of the tendon can lead to conditions that can no longer be sutured. If anything is unclear, we recommend a prompt appointment at a specialised shoulder centre.
- The supraspinatus tendon is the part of the rotator cuff most frequently affected by damage and tears.
- Tears of the supraspinatus tendon cause pain and weaken the strength of the arm to the point of inability to lift the arm against gravity in the event of acute tears of the supraspinatus tendon (pseudoparalysis).
- Persistent pain in the shoulder or upper arm, often associated with excruciating night-time pain.
- As the disease progresses, movement is restricted and even stiffness of the shoulder occurs. Lifting the arm forward or sideways and turning it is difficult.
- Accidents can result in very large cracks which lead to immediate inability to use the shoulder.
- Our shoulder specialist Professor Maier and his team will first carry out a detailed anamnesis with you to record your individual medical history.
- Using special rotator cuff tests, the affected muscles and tendons are then examined in a targeted examination.
- The ultrasound examination allows a dynamic examination of the individual parts of the rotator cuff. Normal x-rays of the shoulder show the condition of the bone structures, and magnetic resonance imaging (MRI) helps to assess the muscles with regard to degenerative changes such as fatty degeneration and to record the entire soft tissue of the shoulder in three dimensions.
- The safest diagnostic method for rotator cuff lesions is arthroscopy of the shoulder. This means that you as the patient receive an anaesthetic and Professor Maier can look into the shoulder joint through a small minimally invasive incision (approx. 5 mm) using a kind of video camera (optics). Because the incision is hardly visible after the scar has healed, we also speak of keyhole technique.
- The advantage of arthroscopy is that your experienced shoulder surgeon at the SSC can use arthroscopy to diagnose the tear and treat it immediately.
- Small tears of the rotator cuffs can be treated well with conservative therapy measures.
- Drugs, autohaemotherapy (ACP), physiotherapy and physical therapy have good results.
- We would be pleased to inform you about the treatment methods in a personal conversation.
- In the case of progressive complaints, after accidents or in the case of competitive athletes, a quick operation is often necessary, as otherwise the cuff will recede, making a suture difficult or impossible.
- The shoulder specialists at the Swabian Joint Center are masters of all surgical techniques and can therefore apply the best surgical method for your shoulder, depending on the degree of damage and location of the rupture.
- The aim of the surgical treatment is the complete refixation of the tendons so that your diseased shoulder regains strength and mobility and becomes pain-free.
- A suture, i.e. a refixation of the tendon to the humerus, is usually possible arthroscopically or using the mini-open technique. Large open therapy procedures are used less and less frequently.
- However, if the patient waits too long and the torn tendon has retracted so far that it can no longer be fixed to the humeral head, the associated muscle becomes fatty and atrophies (atrophy) and suturing is no longer possible. An open muscle-tendon transfer operation can help here if necessary.
- The shoulder is immobilised after the operation using a special positioning cushion so that the tendons grow together without tension.
- After 3 weeks the physiotherapeutic exercises are started.
- Active movements are allowed after suturing the rotator cuff after 6 weeks.
- Full function of the shoulder is usually restored after about six months.
- The end tendons of 4 connected muscles, which surround the head of humerus like a cuff, are called rotator cuffs.
- The muscles of the rotator cuff move from the shoulder blade to the head of humerus and attach their tendons there. The muscles involved are as follows: Subscapular, supraspinatus, infraspinatus and teres minor.
- The rotator cuff cannot be palpated because it is located deep below the shoulder cap muscle (deltoid muscle).
- The rotator cuff stabilises the head of humerus in the small socket at the shoulder joint and is therefore an essential component of pain-free mobility of the upper arm in the shoulder joint.
- For stabilization at the shoulder joint, the strength of a well-trained rotator cuff musculature is required, which is why the shoulder is also referred to as a "friction-locked" joint.
- According to its name, the rotator cuff is responsible for the rotational movement in the shoulder joint in terms of internal and external rotation. A balance of force couples is crucial for pain-free shoulder function.
- A traumatic event or wear and tear due to excessive stress can cause a tear of one or more tendons of the rotator cuff. As a result, the function of the entire shoulder is often impaired.
- The frequency of rotator cuff lesions increases with age.
- The tendons, some of which are overstressed by inflammation, tear, fray and form defects that grow larger and larger.
- In younger people, the most common cause is an accident, in older people degenerative changes in the cuff that lead to a tear.
- If the rotator cuff tendon tears, the supraspinatus tendon is most frequently affected.
- If these defects are diagnosed in time, they can be sutured. If left untreated, the defects often increase further, and regression of the tendon can lead to conditions that can no longer be sutured. If anything is unclear, we recommend a prompt appointment at a specialised shoulder centre.
- The supraspinatus tendon is the part of the rotator cuff most frequently affected by damage and tears.
- Tears of the supraspinatus tendon cause pain and weaken the strength of the arm to the point of inability to lift the arm against gravity in the event of acute tears of the supraspinatus tendon (pseudoparalysis).
- Persistent pain in the shoulder or upper arm, often associated with excruciating night-time pain.
- As the disease progresses, movement is restricted and even stiffness of the shoulder occurs. Lifting the arm forward or sideways and turning it is difficult.
- Accidents can result in very large cracks which lead to immediate inability to use the shoulder.
- Our shoulder specialist Professor Maier and his team will first carry out a detailed anamnesis with you to record your individual medical history.
- Using special rotator cuff tests, the affected muscles and tendons are then examined in a targeted examination.
- The ultrasound examination allows a dynamic examination of the individual parts of the rotator cuff. Normal x-rays of the shoulder show the condition of the bone structures, and magnetic resonance imaging (MRI) helps to assess the muscles with regard to degenerative changes such as fatty degeneration and to record the entire soft tissue of the shoulder in three dimensions.
- The safest diagnostic method for rotator cuff lesions is arthroscopy of the shoulder. This means that you as the patient receive an anaesthetic and Professor Maier can look into the shoulder joint through a small minimally invasive incision (approx. 5 mm) using a kind of video camera (optics). Because the incision is hardly visible after the scar has healed, we also speak of keyhole technique.
- The advantage of arthroscopy is that your experienced shoulder surgeon at the SSC can use arthroscopy to diagnose the tear and treat it immediately.
- Small tears of the rotator cuffs can be treated well with conservative therapy measures.
- Drugs, autohaemotherapy (ACP), physiotherapy and physical therapy have good results.
- We would be pleased to inform you about the treatment methods in a personal conversation.
- In the case of progressive complaints, after accidents or in the case of competitive athletes, a quick operation is often necessary, as otherwise the cuff will recede, making a suture difficult or impossible.
- The shoulder specialists at the Swabian Joint Center are masters of all surgical techniques and can therefore apply the best surgical method for your shoulder, depending on the degree of damage and location of the rupture.
- The aim of the surgical treatment is the complete refixation of the tendons so that your diseased shoulder regains strength and mobility and becomes pain-free.
- A suture, i.e. a refixation of the tendon to the humerus, is usually possible arthroscopically or using the mini-open technique. Large open therapy procedures are used less and less frequently.
- However, if the patient waits too long and the torn tendon has retracted so far that it can no longer be fixed to the humeral head, the associated muscle becomes fatty and atrophies (atrophy) and suturing is no longer possible. An open muscle-tendon transfer operation can help here if necessary.
- The shoulder is immobilised after the operation using a special positioning cushion so that the tendons grow together without tension.
- After 3 weeks the physiotherapeutic exercises are started.
- Active movements are allowed after suturing the rotator cuff after 6 weeks.
- Full function of the shoulder is usually restored after about six months.
Impingement Syndrome

- Impingement syndrome is a synonym for shoulder bottleneck syndrome.
- Due to a bottleneck between the head of the humerus and the acromion, the rotator cuff is clamped between the head of the humerus and the acromion.
- This often leads to degenerative changes, which are associated with pain and limited mobility.
- The impingement leads to a disturbance of the movement and sliding behaviour of the cuff and bony structures can rub against each other and "pinch" the tendon. It becomes inflamed.
- This can cause small cracks in the tendon, which weaken it and can lead to a tendon rupture.
- People who frequently move their arms at shoulder height and above the head for work or sports.
- The syndrome often occurs in competitive athletes such as tennis players, handball and volleyball players, golfers, swimmers and throwing athletes of all kinds.
- The early stage is characterized by acute onset of pain and patients suffer from movement-dependent shoulder pain that occurs in the shoulder joint when the arm is spread.
- Chronic impingement also causes pain at rest, often with pronounced pain at night.
- For a reliable diagnosis of the shoulder impingement syndrome, your shoulder specialist at the Swabian Joint Center will perform various tests, which are supplemented by ultrasound examinations, X-rays or magnetic resonance imaging (MRI).
- At the Swabian Joint Center every impingement syndrome is first treated conservatively, i.e. without surgery.
- In addition to anti-inflammatory, pain-relieving medication and injections, our team of shoulder specialists also uses physiotherapeutic measures.
- The most important therapy for long-term success is active training of the rotator cuff muscles through rotation training. This leads to a re-centring of the head of humerus in the socket and thus to a reduction of the constriction.
- Since the impingement syndrome has developed over many years and a structural adjustment of the complex shoulder mechanics is required, it can take 3 months before the patient is completely free of symptoms with conservative therapy.
- If the conservative treatment measures are not effective or the patient wishes to accelerate the healing process, the shoulder specialists at the Swabian Joint Center can treat impingement syndrome with the help of arthroscopy.
- The operation is performed by means of arthroscopy (joint endoscopy), which means that the patient is given an anaesthetic and the shoulder specialist can look into the shoulder joint through a small minimally invasive incision (approx. 5 mm) using a kind of video camera (optics). Because the incision is hardly visible after the scar has healed, we also speak of keyhole technique.
- The tendon space is expanded by removing bony extensions.
- A possibly inflammatory changed bursa is removed.
- At the same time, the condition of the tendon plate (rotator cuff) is checked.
- In addition, the actual joint space between the head of humerus and the socket is inspected.
- Physiotherapy follows immediately after the impingement operation, which plays an important role in the success of the treatment.
- Specially trained physiotherapists ensure the success of the therapy in this important healing phase.
- After intensive physiotherapy, full mobility of the shoulder is restored 3 months after surgery.
- Impingement syndrome is a synonym for shoulder bottleneck syndrome.
- Due to a bottleneck between the head of the humerus and the acromion, the rotator cuff is clamped between the head of the humerus and the acromion.
- This often leads to degenerative changes, which are associated with pain and limited mobility.
- The impingement leads to a disturbance of the movement and sliding behaviour of the cuff and bony structures can rub against each other and "pinch" the tendon. It becomes inflamed.
- This can cause small cracks in the tendon, which weaken it and can lead to a tendon rupture.
- People who frequently move their arms at shoulder height and above the head for work or sports.
- The syndrome often occurs in competitive athletes such as tennis players, handball and volleyball players, golfers, swimmers and throwing athletes of all kinds.
- The early stage is characterized by acute onset of pain and patients suffer from movement-dependent shoulder pain that occurs in the shoulder joint when the arm is spread.
- Chronic impingement also causes pain at rest, often with pronounced pain at night.
- For a reliable diagnosis of the shoulder impingement syndrome, your shoulder specialist at the Swabian Joint Center will perform various tests, which are supplemented by ultrasound examinations, X-rays or magnetic resonance imaging (MRI).
- At the Swabian Joint Center every impingement syndrome is first treated conservatively, i.e. without surgery.
- In addition to anti-inflammatory, pain-relieving medication and injections, our team of shoulder specialists also uses physiotherapeutic measures.
- The most important therapy for long-term success is active training of the rotator cuff muscles through rotation training. This leads to a re-centring of the head of humerus in the socket and thus to a reduction of the constriction.
- Since the impingement syndrome has developed over many years and a structural adjustment of the complex shoulder mechanics is required, it can take 3 months before the patient is completely free of symptoms with conservative therapy.
- If the conservative treatment measures are not effective or the patient wishes to accelerate the healing process, the shoulder specialists at the Swabian Joint Center can treat impingement syndrome with the help of arthroscopy.
- The operation is performed by means of arthroscopy (joint endoscopy), which means that the patient is given an anaesthetic and the shoulder specialist can look into the shoulder joint through a small minimally invasive incision (approx. 5 mm) using a kind of video camera (optics). Because the incision is hardly visible after the scar has healed, we also speak of keyhole technique.
- The tendon space is expanded by removing bony extensions.
- A possibly inflammatory changed bursa is removed.
- At the same time, the condition of the tendon plate (rotator cuff) is checked.
- In addition, the actual joint space between the head of humerus and the socket is inspected.
- Physiotherapy follows immediately after the impingement operation, which plays an important role in the success of the treatment.
- Specially trained physiotherapists ensure the success of the therapy in this important healing phase.
- After intensive physiotherapy, full mobility of the shoulder is restored 3 months after surgery.
Calcified shoulder

- Calcified shoulder or tendinitis calcarea is the painful accumulation of calcification in a tendon of the rotator cuff on the upper arm.
- It is a disease that progresses in phases and the patients affected often experience severe symptoms caused by a thickening of the tendon under the acromion with symptoms similar to the bottleneck syndrome (impingement syndrome).
- Middle-aged women are often affected. The exact cause of lime deposits is not known.
- Basically, the function of the shoulder joint is restored in the course of the procedure with a reduction in pain.
- Acute stabbing pain in the shoulder.
- The pain becomes worse when lying on the affected shoulder.
- In acute cases, patients are no longer able to lift the arm above shoulder height and complain of severe movement-related pain. These patients need a quick appointment at a specialized shoulder center. [to make an appointment]
- A precise diagnosis of calcified shoulder disease is made by our shoulder specialists at the SGZ through clinical examinations followed by diagnostic equipment such as x-rays, ultrasound and MRT.
- It is important to rule out other causes of shoulder pain such as osteoarthritis or a torn tendon in the rotator cuff.
- With the help of the ultrasound examination, the extent of an additional bursitis can be clearly seen.
- The duration of the disease is not predictable.
- If there is an inflammatory reaction of the lime deposit, it can lead to long lasting, chronic processes.
- Medicated pain therapy
- Targeted injection treatment
- Shockwave therapy
- Individual physiotherapy
- If the success of conservative therapy fails to materialize over a longer period of time, we recommend surgery.
- In the case of the calcified shoulder, the calcified deposits are removed arthroscopically and can thus no longer cause mechanical irritation.
- The minimally invasive procedure of arthroscopy protects the surrounding structures and the intervention is less stressful and less risky for the body.
- After the operation the shoulder may be actively moved.
- Individual physiotherapy with training of the muscles of the rotator cuff is important.
- The ability to work is restored after 4-6 weeks, depending on the profession.
- Calcified shoulder or tendinitis calcarea is the painful accumulation of calcification in a tendon of the rotator cuff on the upper arm.
- It is a disease that progresses in phases and the patients affected often experience severe symptoms caused by a thickening of the tendon under the acromion with symptoms similar to the bottleneck syndrome (impingement syndrome).
- Middle-aged women are often affected. The exact cause of lime deposits is not known.
- Basically, the function of the shoulder joint is restored in the course of the procedure with a reduction in pain.
- Acute stabbing pain in the shoulder.
- The pain becomes worse when lying on the affected shoulder.
- In acute cases, patients are no longer able to lift the arm above shoulder height and complain of severe movement-related pain. These patients need a quick appointment at a specialized shoulder center. [to make an appointment]
- A precise diagnosis of calcified shoulder disease is made by our shoulder specialists at the SGZ through clinical examinations followed by diagnostic equipment such as x-rays, ultrasound and MRT.
- It is important to rule out other causes of shoulder pain such as osteoarthritis or a torn tendon in the rotator cuff.
- With the help of the ultrasound examination, the extent of an additional bursitis can be clearly seen.
- The duration of the disease is not predictable.
- If there is an inflammatory reaction of the lime deposit, it can lead to long lasting, chronic processes.
- Medicated pain therapy
- Targeted injection treatment
- Shockwave therapy
- Individual physiotherapy
- If the success of conservative therapy fails to materialize over a longer period of time, we recommend surgery.
- In the case of the calcified shoulder, the calcified deposits are removed arthroscopically and can thus no longer cause mechanical irritation.
- The minimally invasive procedure of arthroscopy protects the surrounding structures and the intervention is less stressful and less risky for the body.
- After the operation the shoulder may be actively moved.
- Individual physiotherapy with training of the muscles of the rotator cuff is important.
- The ability to work is restored after 4-6 weeks, depending on the profession.
Shoulder dislocation

- The shoulder dislocation describes the dislocation of the shoulder joint.
- After the joint has been set, there is usually instability in the shoulder joint.
- Shoulder instability can manifest itself in several directions.
- The most common cause of shoulder dislocation is an accident and the humeral head is dislocated forward and downward.
- In acute cases, a fracture of the humerus must be ruled out, e.g. by means of an x-ray, before the patient is able to set it.
- Even after the humeral head has been repositioned, a feeling of instability can remain, so that the shoulder can no longer be fully loaded.
- Capsule injuries and labrum lesions (injury to the joint lip) can be diagnosed with magnetic resonance imaging (MRI).
- Traumatic shoulder dislocation due to an accident or sports injury is the most common form.
- Posttraumatic, recurrent shoulder dislocation means that dislocations of the shoulder joint occur again and again after a first accidental event, often during minor movements such as sleep. are predispositions:
- Injury of the acetabular rim (= Bankart lesion)
- Extended joint capsule
- Damage to capsule and ligament structures
- Impression lesion on the humeral head (= Hill-Sachs lesion)
- Habitual shoulder dislocation means that a malformation or acquired malposition of the shoulder joint constantly leads to shoulder dislocation. Sometimes the cause is also a general muscle or ligament weakness.
- Feeling of instability
- Pain-related movement restriction
- Loss of function
- Once the fracture has been ruled out, the shoulder is repositioned (settling), possibly with analgosedation.
- After reduction, the blood circulation, motor function and sensation on the affected arm are checked, and an X-ray is also taken.
- Immobilization of the arm is recommended for a maximum of 1 week and a quick presentation to the specialized shoulder surgeon for further clarification should be made.
- At the Swabian Joint Center, the shoulder is reduced by the specialized shoulder team around Professor Maier using the method described by Arlt. You as the patient sit on a chair and let the affected, dislocated arm hang over a padded backrest.
- It is important that you try to relax so that the muscles that surround your shoulders become loose.
- If necessary, the shoulder specialist may have to provide support in the form of medication (analgosedation).
- The shoulder specialist must not make any jerky movements here ("Hollywood movie style").
- Reduction is achieved by gentle, slow longitudinal traction on the arm with the elbow bent at 90° and slight abduction (spreading) of the arm. The longitudinal traction can be supplemented by gentle rotational movements.
- After the medical history and physical examination, the X-ray examination excludes a fracture.
- Ultrasound and magnetic resonance imaging (MRI) can reveal the full extent of the injury to the capsule, ligament structures and joint lip, and accompanying injuries can be ruled out.
- Fracture: Tuberculum majus tear, bony Bankart lesion
- Hill-Sachs lesion: increased risk of recurrence depending on size
- Reverse Hill-Sachs lesion: increased risk of recurrence depending on size
- Bankart lesion: lesion of the anterior-inferior labrum glenoidale → Increased risk of recurrence
- Other possible injuries of the capsular labrum complex and the glenohumeral ligaments
- SLAP lesion (Superior Labrum Anterior to Posterior)
- ALPSA lesion (Anterior Labroligamentous
Periosteal Sleeve Avulsion) - HAGL lesion (Humeral Avulsion of Glenohumeral Ligament)
- GLAD lesion (Glenolabral Articular Disruption)
- Rotator cuff injury: 40% of patients over 40 years of age have a rotator cuff injury
- Nerve and vessel injuries
- There is a high risk of recurrence of shoulder dislocation after the initial event, depending on the patient's age and type of dislocation.
- The question of whether surgery is necessary depends on the concomitant injuries, the patient's age and the sporting requirements.
- The operation is performed in the case of initial traumatic luxations in young, demanding patients without hyperlaxity or significant accompanying bony injuries.
- Recurrent dislocations in older patients are also treated surgically.
- More severe cases, particularly pronounced torn ligaments and severe shoulder instabilities make the operation necessary.
- After a shoulder dislocation operation, the shoulder is initially immobilised.
- Intensive physiotherapy usually begins after 14 days.
- It then takes 8-12 weeks until the full mobility of the shoulder is restored.
- The shoulder dislocation describes the dislocation of the shoulder joint.
- After the joint has been set, there is usually instability in the shoulder joint.
- Shoulder instability can manifest itself in several directions.
- The most common cause of shoulder dislocation is an accident and the humeral head is dislocated forward and downward.
- In acute cases, a fracture of the humerus must be ruled out, e.g. by means of an x-ray, before the patient is able to set it.
- Even after the humeral head has been repositioned, a feeling of instability can remain, so that the shoulder can no longer be fully loaded.
- Capsule injuries and labrum lesions (injury to the joint lip) can be diagnosed with magnetic resonance imaging (MRI).
- Traumatic shoulder dislocation due to an accident or sports injury is the most common form.
- Posttraumatic, recurrent shoulder dislocation means that dislocations of the shoulder joint occur again and again after a first accidental event, often during minor movements such as sleep. are predispositions:
- Injury of the acetabular rim (= Bankart lesion)
- Extended joint capsule
- Damage to capsule and ligament structures
- Impression lesion on the humeral head (= Hill-Sachs lesion)
- Habitual shoulder dislocation means that a malformation or acquired malposition of the shoulder joint constantly leads to shoulder dislocation. Sometimes the cause is also a general muscle or ligament weakness.
- Feeling of instability
- Pain-related movement restriction
- Loss of function
- Once the fracture has been ruled out, the shoulder is repositioned (settling), possibly with analgosedation.
- After reduction, the blood circulation, motor function and sensation on the affected arm are checked, and an X-ray is also taken.
- Immobilization of the arm is recommended for a maximum of 1 week and a quick presentation to the specialized shoulder surgeon for further clarification should be made.
- At the Swabian Joint Center, the shoulder is reduced by the specialized shoulder team around Professor Maier using the method described by Arlt. You as the patient sit on a chair and let the affected, dislocated arm hang over a padded backrest.
- It is important that you try to relax so that the muscles that surround your shoulders become loose.
- If necessary, the shoulder specialist may have to provide support in the form of medication (analgosedation).
- The shoulder specialist must not make any jerky movements here ("Hollywood movie style").
- Reduction is achieved by gentle, slow longitudinal traction on the arm with the elbow bent at 90° and slight abduction (spreading) of the arm. The longitudinal traction can be supplemented by gentle rotational movements.
- After the medical history and physical examination, the X-ray examination excludes a fracture.
- Ultrasound and magnetic resonance imaging (MRI) can reveal the full extent of the injury to the capsule, ligament structures and joint lip, and accompanying injuries can be ruled out.
- Fracture: Tuberculum majus tear, bony Bankart lesion
- Hill-Sachs lesion: increased risk of recurrence depending on size
- Reverse Hill-Sachs lesion: increased risk of recurrence depending on size
- Bankart lesion: lesion of the anterior-inferior labrum glenoidale → Increased risk of recurrence
- Other possible injuries of the capsular labrum complex and the glenohumeral ligaments
- SLAP lesion (Superior Labrum Anterior to Posterior)
- ALPSA lesion (Anterior Labroligamentous
Periosteal Sleeve Avulsion) - HAGL lesion (Humeral Avulsion of Glenohumeral Ligament)
- GLAD lesion (Glenolabral Articular Disruption)
- Rotator cuff injury: 40% of patients over 40 years of age have a rotator cuff injury
- Nerve and vessel injuries
- There is a high risk of recurrence of shoulder dislocation after the initial event, depending on the patient's age and type of dislocation.
- The question of whether surgery is necessary depends on the concomitant injuries, the patient's age and the sporting requirements.
- The operation is performed in the case of initial traumatic luxations in young, demanding patients without hyperlaxity or significant accompanying bony injuries.
- Recurrent dislocations in older patients are also treated surgically.
- More severe cases, particularly pronounced torn ligaments and severe shoulder instabilities make the operation necessary.
- After a shoulder dislocation operation, the shoulder is initially immobilised.
- Intensive physiotherapy usually begins after 14 days.
- It then takes 8-12 weeks until the full mobility of the shoulder is restored.
Shoulder arthrosis - Omarthrosis

- Shoulder arthrosis (omarthrosis) means that there has been wear and tear of the joint cartilage of the shoulder.
- As a result, the head of humerus becomes increasingly rounded and the soft tissue structures are shortened with painful restriction of joint movement.
- Other causes of shoulder arthrosis are necrosis of the humeral head, rheumatism, post-traumatic shoulder injuries and chronic shoulder dislocation (instability arthrosis).
- Movement-dependent pain when lifting the arm, which increases under load
- Frequent pain at rest and at night
- Restriction of activities of daily living
- The anamnesis provides the shoulder specialists at the Swabian Joint Center with the decisive indications of shoulder arthrosis.
- The X-ray examination shows the reduction of the joint space caused by the wear and tear of the cartilage.
- Ultrasound examination and magnetic resonance imaging (MRI) show accompanying damage to muscles, tendons and ligaments.
- Computer tomography shows the exact extent of the joint changes, such as bony changes to the socket, which is important for later 3D surgery planning.
- In the initial stages, pain and any inflammation can be treated by means of targeted drug therapy.
- Electrotherapy, heat or cold applications and also acupuncture are used for painful movement restrictions and muscle tension.
- In the case of advanced shoulder arthrosis, targeted injections of cortisone into the focus of inflammation can relieve the pain.
- Hyaluronic acid therapy and autohaemotherapy (ACP) can improve the lubrication of the shoulder joint, which can delay the progression of the disease.
- Surgery is required when there has been final wear and tear in the shoulder joint and conservative therapy no longer provides relief.
- A pronounced loss of function with complete loss of the ability to perform the activities of daily living and bony deformities make surgery necessary.
- Your individual level of suffering is decisive for the right time of operation.
- In the case of end-stage shoulder arthrosis, the implantation of an artificial joint of the shoulder (endoprosthetic replacement) is the therapy of choice.
- An individual 3D planning is carried out for each patient before the operation.
- Whereas artificial joint operations on the shoulder used to lag behind the development of prostheses for the hip and knee joint, modern implant systems for the shoulder are now so well developed that excellent results can be achieved with the right implantation and correct implant selection.
- In Germany, shoulder joint replacement is performed about 10 times less frequently than hip joint replacement.
- For this reason, it is essential that the presentation be made at a specialised shoulder centre before the operation.
- It has been scientifically proven that the surgeon who performs the procedure frequently and routinely with his team has better results and a lower complication rate.
- Patients are hospitalized for about 4 days after shoulder joint replacement. During the inpatient stay, targeted physiotherapy begins.
- The loss of pain and the improvement of shoulder function are usually so good after shoulder joint replacement that sporting activity can also be resumed after intensive rehabilitation.
- Fitness, Nordic walking, hiking, tennis and golf are among the possible sports.
- Full mobility of the shoulder is usually restored after 3 months.
- We recommend clinical and radiological follow-up after 1, 3, 5 years and then every 5 years.
- Shoulder arthrosis (omarthrosis) means that there has been wear and tear of the joint cartilage of the shoulder.
- As a result, the head of humerus becomes increasingly rounded and the soft tissue structures are shortened with painful restriction of joint movement.
- Other causes of shoulder arthrosis are necrosis of the humeral head, rheumatism, post-traumatic shoulder injuries and chronic shoulder dislocation (instability arthrosis).
- Movement-dependent pain when lifting the arm, which increases under load
- Frequent pain at rest and at night
- Restriction of activities of daily living
- The anamnesis provides the shoulder specialists at the Swabian Joint Center with the decisive indications of shoulder arthrosis.
- The X-ray examination shows the reduction of the joint space caused by the wear and tear of the cartilage.
- Ultrasound examination and magnetic resonance imaging (MRI) show accompanying damage to muscles, tendons and ligaments.
- Computer tomography shows the exact extent of the joint changes, such as bony changes to the socket, which is important for later 3D surgery planning.
- In the initial stages, pain and any inflammation can be treated by means of targeted drug therapy.
- Electrotherapy, heat or cold applications and also acupuncture are used for painful movement restrictions and muscle tension.
- In the case of advanced shoulder arthrosis, targeted injections of cortisone into the focus of inflammation can relieve the pain.
- Hyaluronic acid therapy and autohaemotherapy (ACP) can improve the lubrication of the shoulder joint, which can delay the progression of the disease.
- Surgery is required when there has been final wear and tear in the shoulder joint and conservative therapy no longer provides relief.
- A pronounced loss of function with complete loss of the ability to perform the activities of daily living and bony deformities make surgery necessary.
- Your individual level of suffering is decisive for the right time of operation.
- In the case of end-stage shoulder arthrosis, the implantation of an artificial joint of the shoulder (endoprosthetic replacement) is the therapy of choice.
- An individual 3D planning is carried out for each patient before the operation.
- Whereas artificial joint operations on the shoulder used to lag behind the development of prostheses for the hip and knee joint, modern implant systems for the shoulder are now so well developed that excellent results can be achieved with the right implantation and correct implant selection.
- In Germany, shoulder joint replacement is performed about 10 times less frequently than hip joint replacement.
- For this reason, it is essential that the presentation be made at a specialised shoulder centre before the operation.
- It has been scientifically proven that the surgeon who performs the procedure frequently and routinely with his team has better results and a lower complication rate.
- Patients are hospitalized for about 4 days after shoulder joint replacement. During the inpatient stay, targeted physiotherapy begins.
- The loss of pain and the improvement of shoulder function are usually so good after shoulder joint replacement that sporting activity can also be resumed after intensive rehabilitation.
- Fitness, Nordic walking, hiking, tennis and golf are among the possible sports.
- Full mobility of the shoulder is usually restored after 3 months.
- We recommend clinical and radiological follow-up after 1, 3, 5 years and then every 5 years.
